Background: Myelodysplastic neoplasms (MDS) are a clonal, heterogenic disease of the hematopoietic stem cell. Pathophysiology is mainly related to intrinsic myeloid abnormalities, epigenetic changes and immune system deregulation that leads to changes in the bone marrow microenvironment. MDS patients have shown broad and heterogenic changes in cytokine concentrations compared to controls. An elevation of pro-apoptotic and inflammatory cytokines and chemokines has been described. Nevertheless, the role of inflammatory soluble factors is still poorly understood. We aim to describe cytokine concentrations in the bone marrow of MDS patients and how it correlates with the immune population and clonal hematopoiesis.
Methods: We prospectively analyzed 60 bone marrow plasma samples. Forty-four MDS patients without RS or 5q deletion, 8 healthy donors (HD) and 9 cytopenia of unknown significance (CUS). Cytokine/chemokine concentration were analyzed with ThermoFisher commercial kit ProcartaPlexTM Multiplex immunoassay of 32-PLEX (EGF/eotaxin/FGF-2/G-CSF/GM-CSF/HGF/INFalpha/ IFNgamma/IL-1alpha,/IL1-b/IL-10/IL-12/IL-13/IL-15/IL-17a/IL-1RA/IL-2/IL-22 /IL3 /IL-4/IL-5/IL-6/IL-7/IL-8/IL-9), carried out by Luminex® platform. Furthermore, we analyzed NK subpopulations differentiating an immature population (CD56 brigthCD16 −) from a mature one (CD56 dimCD16+). Lymphocyte T sub-populations were studied in PB samples determined as CD45+CD3+ and the different expression of the following monoclonal antibodies CD4/CD8/CCR7/CD45RA/CD27/CD28/CD25/CD127/CXCR3/CXCR6. The analysis was performed, by flow cytometry, on fresh samples, following a membrane staining protocol with 10-colors/3 lasers. Finally, molecular analysis was performed by NGS using the Oncomine Myeloid Research Assay included 40 genes.
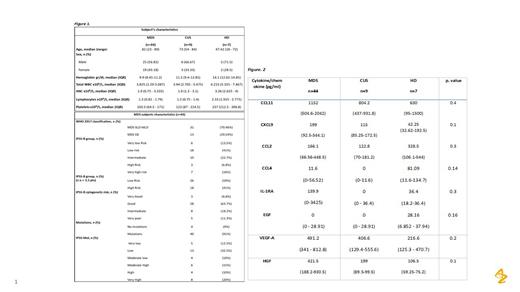
Results: A total of 60 subjects were included (median age was 71 years-old and 35% were female). Auto-immune disease was present in 6.6% (Figure 1). Regarding chemokines, CCL11 a pro-inflammatory chemokine was increased in MDS (59.73pg/ml) compared to CUS (41.24pg/ml) and HD (22.63pg/ml), also CXCL9, with a complex role in tumor progression, being 29.08pg/ml in MDS, 17.14pg/ml in CUS and 1.13pg/ml in HD. On the other hand, CCL2 and CCL4 showed lower concentrations in MDS vs HD but higher than CUS (Figure 2). Interleukins analysis showed, IL-1RA higher concentrations in MDS (139.9pg/ml), than HD (36.4pg/mL) and no detection in CUS. IL- 2 was detected only in HD (7.61pg/mL) and IL-3 showed greater concentrations in HD and CUS (20.75pg/ml) compared to MDS (13.84pg/ml). IL-6 did not showed differences among the three groups; in 18.3% subjects (11/60) concentrations were ≥10pg/ml and 8 were MDS. IL-8, a pro-inflammatory/proangiogenic cytokine, showed increased concentrations in only 23% subjects (14/60); 13 were MDS. Regarding growth factors, we observed EGF only in HD (28.16%), whilst HGF and VEGF-A showed higher concentrations in MDS.
Mature NK sub-populations were increased in CUS (76.16%) vs MDS (11.58%), (p=0.006) and HD (10.66%), (p=0.01). Moreover, CD8+ T lymphocytes between CUS 49.79% vs MDS 14.29% and HD 1.68 (p=0.05) and Th2 in MDS of 22.71% vs CUS 17.5 (p=0.031) without differences to HD 22.54%.
Forty-six MDS subjects presented ≥3 somatic mutations, those presented higher concentrations of CCL11 (73.56pg/mL), HGF (497.7pg/mL), CCL2 (95.3pg/ml) and VEGF-A (506pg/mL). Interestingly, we found that among CUS subjects 66.6% (6/9) presented mutations, 2 DMT3A (VAF < 5%), 1 IDH1 (VAF 3.7%), 1 SRSF2 (VAF 38.9%), 1 TET2 (VAF 39.5%), 1 ZRSR2 (VAF 35%), 1 PHF6 (VAF 39.8%).
Finally, regarding IPSS-R risk, we observed higher concentrations of inhibitory proteins like IL-10 and cytokines involved in the regulation of tumor microenvironment like CXCL10 or CCL2 in HR-MDS, while in LR-MDS we observed a more cytotoxic and inflammatory profile (Figure 2).
Conclusions: Our study describes a heterogenic background of MDS. Suggesting an increase in some cytokines related to cell recruitment, migration, and proliferation in the bone marrow of MDS and an exhaustive and inhibitory environment in those patients with high-risk characteristics, pointing out the important role of immune subpopulations and environment in the clonal progression.
Disclosures
Molero Yordi:Jazz Pharmaceuticals: Honoraria; Novartis: Honoraria; BMS: Honoraria; BioTest: Honoraria; Gilead: Honoraria; AstraZeneca: Current Employment; Oryzon Genomics S.A.: Consultancy. Pierola:Astra Zeneca: Research Funding; Astellas: Consultancy; Syros: Consultancy, Speakers Bureau; BMS: Consultancy, Speakers Bureau; Jazz Pharma: Consultancy, Speakers Bureau; Abbvie: Speakers Bureau; Novartis: Speakers Bureau. Diez-Campelo:Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead Sciences: Other: Travel expense reimbursement; BMS/Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Advisory board fees; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees. Salamero:Pfizer: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Jazz: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal